There is little doubt that the expanded Medicaid program for low-income adults under the Affordable Care Act is proving to be far more costly than originally billed by the administration.
The latest Medicaid actuarial report issued late last month pegged the per enrollee cost for adults at $6,366 in 2015, up 49 percent from previous estimates. Over the coming decade, Medicaid outlays through this program will be nearly $250 billion higher than previous actuarial projections.
That trend could pose serious financial challenges for the federal government, which is currently footing the cost, and the more than 30 states that have opted into the program so far that eventually must pick up ten percent or more of the overall cost of the expanded health insurance.
Related: Governor Takes Aim at Kentucky’s Medicaid Expansion Program
At the same time, the societal, public health and economic benefits of providing millions of previously uninsured low income adults with health care coverage are substantial, as a new Harvard University school of public health study clearly documents.
The study focused on Kentucky and Arkansas -- two of the states where Medicaid coverage was expanded under the Affordable Care Act during the past two years despite considerable political turbulence -- and Texas, where state officials rejected participation in the program. The Supreme Court left it up to the states to decide whether to take part in the program, and many states controlled by Republicans who oppose Obamacare have rejected the offer.
The study, published on Monday in JAMA Internal Medicine, concludes that low-income adults in Kentucky and Arkansas received far more primary and preventative care, made fewer visits to hospital emergency rooms, and in general experienced much improved health when compared to low-income adults living in Texas.
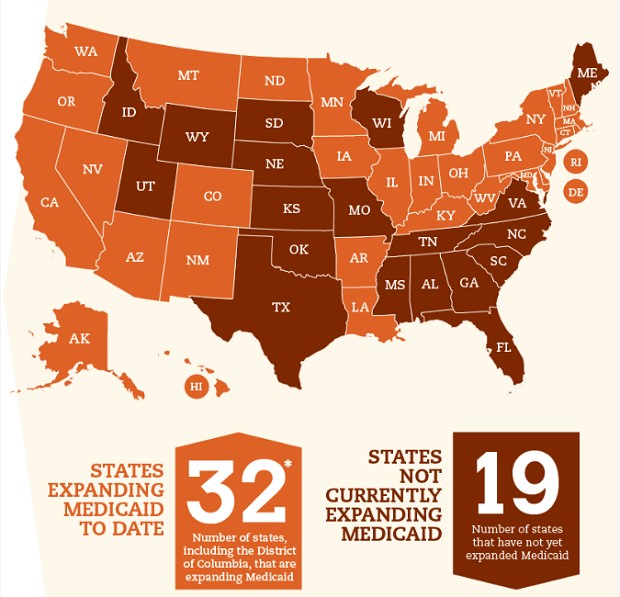
Source: FamiliesUSA.org
In targeting Kentucky and Arkansas for the study, the Harvard researchers chose two of the most controversial programs in the country.
Kentucky Gov. Matt Bevin campaigned on a pledge to dismantle his state’s highly successful Medicaid expansion program, but backed down after taking office in January. Still, the Tea Party Republican is pressing for major changes that would toughen eligibility, slash benefits, impose new fees and force tens of thousands of people out of the program.
Related: Get Ready for Huge Obamacare Premium Hikes in 2017
Earlier this year, Republican Gov. Asa Hutchinson of Arkansas pushed through legislation that scrapped a “private option” approach to Medicaid expansion, replacing it with an alternative called Arkansas Works. The new approach includes small premiums for people earning between 100 and 138 percent of the federal poverty level and an end to retroactive coverage.
Both Bevin and Hutchinson need waivers from the federal government to implement their new plans.
Harvard researchers interviewed about 9,000 low-income adults in the three states between late 2013 and the end of 2015. Among the study’s most dramatic findings:
* The uninsured rate declined from 42 percent to 14 percent in Arkansas and from 40 percent to 9 percent in Kentucky, while the rate dropped far less in Texas, from 39 percent to 32 percent.
* There was a direct correlation between Medicaid expansion and access to primary care, reduced likelihood of emergency room visits, more affordable medication, and reduced out-of-pocket spending by people who are barely above the poverty level.
* Substantial numbers of adults in Kentucky and Arkansas took advantage of screening and treatment for diabetes and other chronic illnesses. Quality of care ratings improved dramatically while more and more adults reported improvement in their health.
The research team said it documented similar benefits for low-income adults in Kentucky and Arkansas, despite the fact that the two states adopted different approaches to providing expanded Medicaid coverage.
"What this means is that it doesn't matter so much how states expand coverage," Benjamin Sommers, assistant professor of health policy and economics at the Harvard Chan School of public health and assistant professor of medicine at Harvard Medical School, said in a statement. "What matters is whether they expand at all."
Related: More Bad News for the Remaining Obamacare Co-ops
Not surprisingly, earlier academic studies of the impact of expanded Medicaid showed increased affordability and access to health care, as low income adults who have struggled to get by without health insurance rushed to sign up for the new government coverage. Yet those earlier findings from 2014 and early 2015 showed expanded Medicaid coverage had relatively limited impact on utilization, preventative care and general health conditions, according to Sommers.
However, more recent data gathered by Harvard shows that many beneficiaries are more aggressively taking advantage of the health care coverage – a positive sign suggesting that the program is fostering a heathier and presumably more productive segment of society. As more people take advantage of expanded Medicaid, hospitals and state and local governments are under less pressure to provide costly emergency coverage. Moreover, healthier Americans have a better chance of finding and keeping jobs, rather than relying heavily on government social safety net programs like food stamps and unemployment checks.
"Health insurance matters to people's health," Sommers, the chief author of the new study, said in his statement. "Our study shows that with health insurance, whether it's Medicaid or private coverage, people can better afford their medical care, get more preventive care and chronic disease management, and ultimately achieve better overall health."
The study notes that the Obama administration has allowed demonstration waivers to push Medicaid toward an alternative health care model which stresses private insurance markets, premium assistance, market competition, individual choice and patient cost sharing to bring down overall costs. The push toward Medicaid premium assistance is especially important in attempting to encourage doctors to treat more Medicaid patients – and get more bang from the Medicaid buck.
Right now, Medicaid reimbursement rates are far below those of Medicare and employer provided insurance, and doctors often refuse to see Medicaid patients. But premium assistance is costly, and the Government Accountability Office has questioned whether such a waiver is budget neutral, which is a federal requirement.





