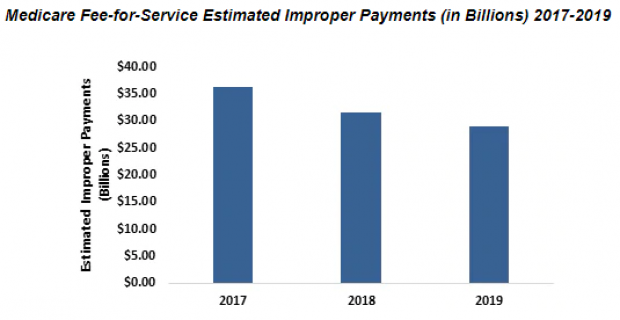
The Centers for Medicare & Medicaid Services announced Monday that the improper payment rate for traditional Medicare fell in fiscal year 2019 to 7.25%, down from 8.12% in fiscal year 2018 and its lowest level since 2010. Improper payments by the Medicare fee-for-service program were $28.9 billion, down $7 billion from fiscal 2017.
CMS attributed the decline to its policy clarifications and changes to required documentation along with aggressive efforts to reduce fraud. CMS also noted that improper payments are not necessarily a measure of fraud. The term refers to government payments that should not have been made or were made in incorrect amounts (both overpayments and underpayments).
“CMS has taken a multifaceted approach that includes provider enrollment and screening standards to keep bad actors out of the program, enforcement against bad actors, provider education on our rules and requirements, and advanced data analytics to stop improper payments before they happen,” CMS Administrator Seema Verma said. “These initiatives strike an important balance between preventing improper payments and reducing the administrative burden on legitimate providers and suppliers.”
CMS estimated that improper Medicaid payments for fiscal 2019 totaled $57.4 billion (a 14.9% rate) and $2.7 billion for the Children’s Health Insurance Program (a 15.8% rate). Its report warned of “high levels of observed eligibility errors,” noting that the data raised concerns about the number of people enrolled in Medicaid who might not qualify for the program or have not provided sufficient documentation.