As states start enforcing more restrictive pre-pandemic rules in their Medicaid programs, data collected by the health care foundation KFF shows considerable variation across states in the percentage of participants being disenrolled, with thousands of people losing health care for procedural reasons such as failing to complete paperwork.
Not all states have started the disenrollment process, and not all of those that have are releasing data, but the 11 states analyzed by KFF – Florida, Arkansas, Indiana, Arizona, New Hampshire, Virginia, South Dakota, Iowa, Idaho, Pennsylvania and Nebraska – have removed more than 500,000 people from their Medicaid programs so far. About half of those disenrollments were in Florida alone.
The rate of disenrollment in each state varies considerably. At the high end, Florida has removed 54% of beneficiaries reviewed so far, and Arkansas has removed 51%. At the other extreme, Pennsylvania and Virginia have removed just 10% of those reviewed. The median disenrollment rate in the 9 states that provide sufficient data is 24%.
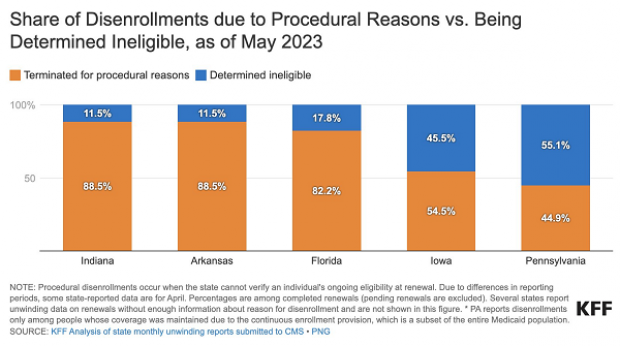
Of particular concern is the number of people who are being removed from Medicaid for procedural reasons, which occurs when states cannot determine the eligibility of a beneficiary, typically due to incomplete paperwork. In both Indiana and Arkansas, more than 88% of disenrollments have been procedural. In Florida, 82.2% of disenrollments are procedural, while in Iowa, the number is 54.4%.
Overall, the data suggest that most people who have been removed from Medicaid so far have been disenrolled for procedural reasons.
While some people who have been disenrolled may no longer be eligible to remain on Medicaid, KFF analysts say many probably are. “High procedural disenrollments raise concerns particularly in light of recent findings from a KFF survey that nearly two-thirds of current Medicaid enrollees said they did not have a change in income or circumstance in the past year that would make them ineligible for Medicaid,” KFF analysts wrote Tuesday. “While it is possible that some people are not completing the renewal process because they have other coverage, the survey findings suggest many of the people whose coverage was terminated for procedural reasons in the past month likely remain eligible.”
Washington Post columnist Catherine Rampell said the data points to a “scandalous” degree of government ineptitude. “Based on available data, majority of Americans losing their Medicaid coverage as part of the national ‘unwinding’ are being disenrolled for paperwork reasons -- *not* because they were actually reassessed & determined ineligible for coverage,” Rampell tweeted Thursday. “These people are losing insurance not because their incomes rose, or they aged out of a program. Rather, they’re losing coverage for pointless bureaucratic reasons, like state sending mail to [the] wrong address.”