Americans continue to lose the battle of the bulge.
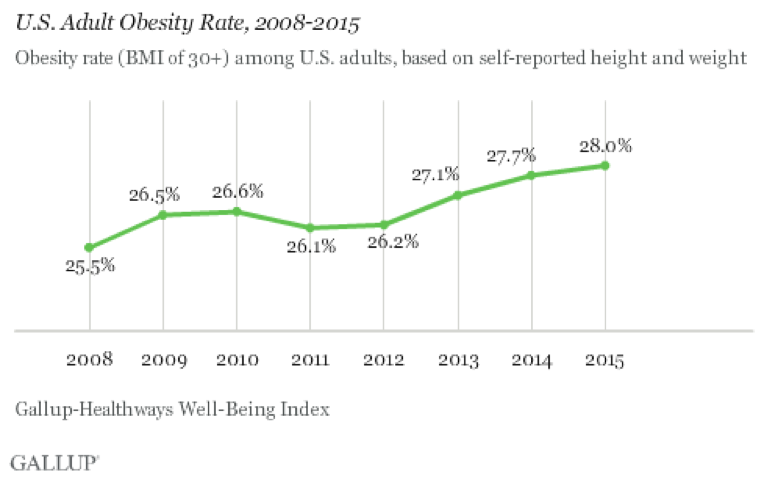
A new Gallup survey published on Friday shows that the obesity rate among adults surged in 2015 to a new high of 28 percent, or a 2.5 percentage point increase since 2008. That means the ranks of dangerously overweight Americans increased by 6.1 million adults over that seven-year period.
Related: Why Obese Mothers Are More Likely to Have Autistic Children
Obesity is fast becoming the top health threat in this country. It consumes hundreds of billions of dollars annually in treatment of related chronic conditions, including diabetes, hypertension and heart disease, as well as declining productivity and depressed wages dues to lost time at work.
An analysis prepared for The Fiscal Times in 2014 by Scott Kahan, director of the National Center for Weight & Wellness at George Washington University, estimated the yearly cost of obesity at $305.1 billion. That included direct medical and non-medical services, worker productivity losses, disability issues and premature death. The overall cost has continued to mount.
Besides the more than one quarter of U.S. adults who are deemed obese, an additional 35.6 percent of adults are classified as overweight. Only 35.6 percent of Americans are of “normal weight,” based on Gallup’s Body Mass Index calculations using self-reported survey data on height and weight.
Previous studies have shown that the rate of dangerously overweight Americans increased the most among people over the age of 65 — with women showing greater problems with weight gains than men. Moreover, African Americans struggled far more than whites and Asian Americans in dealing with obesity.
Related: Budget Busting U.S. Obesity Costs Climb Past $300 Billion a Year
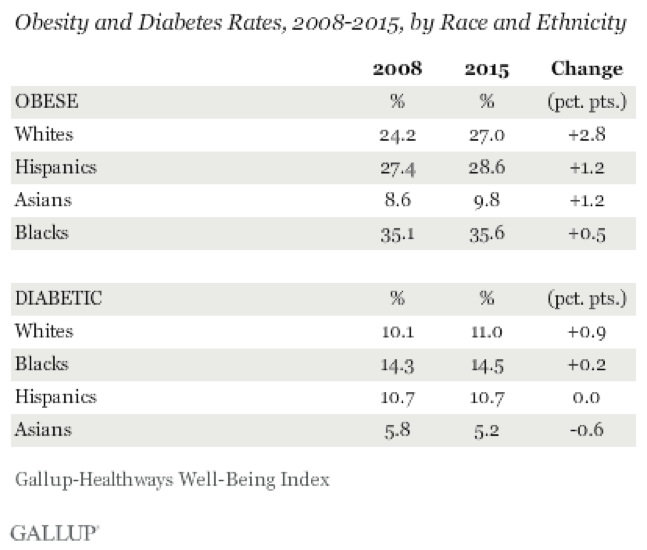
But in the latest Gallup findings, based on interviews with hundreds of thousands of people, while blacks continue to suffer disproportionately from obesity and diabetes, the sharpest increase in the rates of those conditions since 2008 was among white adults.
Twenty-seven percent of white respondents reported problems of obesity in 2015, a net increase of 2.8 percentage points. By comparison, 35.6 percent of African American respondents said they were obese in 2015, but that was only a net increase of 0.5 percent over 2008.
“Across racial and ethnic groups, increases in obesity and diabetes rates since 2008 have been uneven,” Gallup reported. “Both rates have increased much more among whites than among blacks, Asians and Hispanics.”
The Gallup study didn’t offer an explanation for this changing dynamic. However, the report comes on the heels of findings last November by two prominent Princeton University researchers of a marked increase in the mortality rate of middle-aged white (non-Hispanic) men and women between 1999 and 2013.
Related: U.S. Obesity Rate Hits a Costly New High
That change represented a reversal of decades of progress in extending the lives of middle-aged whites and pointed to “growing distress in this population,” according to the study.
By analyzing health and mortality data from the Centers for Disease Control and Prevention and from other sources, researchers Angus Deaton and Anne Case concluded that climbing death rates among middle-aged whites were being caused by an epidemic of suicides and health problems stemming from substance abuse, including alcoholic liver disease and overdoses of heroin and prescription drugs.
Related: How the Obesity Epidemic Drains Medicare and Medicaid
Binge drinking and an unhealthy life style can contribute to problems of obesity. Nearly 40 percent of adults ages 40 to 59 were obese as of 2011, according to a 2015 study by the Robert Wood Johnson Foundation.
The new Gallup report concluded by saying that states, communities and workplaces can all develop intervention programs linked to reducing obesity. “While exercise, produce consumption and healthy eating are all important factors, less obvious aspects of poor well-being are also key predictors of its occurrence, including smoking, depression, food insecurity, not having a safe place to exercise [and] not having a personal doctor.”





