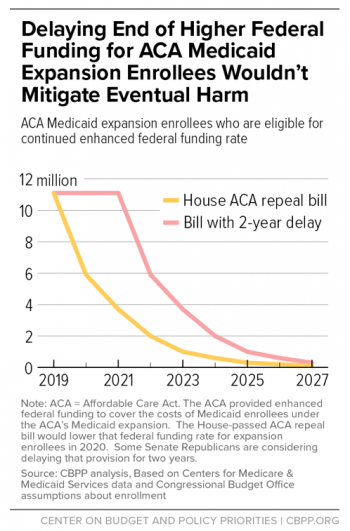
A plan being discussed by Senate Republicans that would sand down some of the rough edges of the House-passed American Health Care Act’s Medicaid reductions would only postpone the disruption awaiting some Americans who benefited from the Affordable Care Act’s Medicaid expansion, a new analysis shows. And it wouldn’t postpone it for very long, at that.
As part of a move to cut some $834 billion in Medicaid spending over a decade, the AHCA would drastically shrink the federal subsidy that goes to states that agreed to expand
eligibility for the program to childless, able-bodied adults who are not yet eligible for Medicaid. Under current law, the federal government pays 90 percent of the cost of coverage for individuals who joined the program under the expansion.Related: GOP Struggles to Explain AHCA’s $880 Billion Medicaid Cuts
The AHCA would change that formula, bringing the reimbursement rate for states down to the matching rate that applies to individuals eligible for the program under the old rules. That percentage varies by state, but the average rate is 57 percent of costs.
The result of such a move, claim Matt Broaddus and Edwin Park of the left-leaning Center on Budget and Policy Priorities, would be an enormous new financial burden on most of the states that expanded Medicaid under the ACA -- one that many of them would be unwilling or unable to shoulder. The result is that a large percentage of the 11 million Americans who, at any given time, have health coverage because of the Medicaid expansion would likely lose it.
“By eliminating the enhanced federal funding for new enrollees, the AHCA would require states either to sharply increase their own spending or to end the expansion,” they write. “States’ costs for the expansion population would more than triple by 2021; they would increase by an estimated $20.6 billion, or 206 percent, across the expansion states in 2021 alone. The higher costs would range from an estimated 104 percent increase in state funding for the expansion population in West Virginia to a 262 percent increase in Massachusetts.”
GOP members of the Senate are looking at ways to do away with the higher funding for Medicaid without appearing heartless -- or at least by pushing the consequences past the next presidential election.
Related: Republicans Eye Medicaid Cuts to Help Finance Their New Health Plan
One such plan would phase in the reduction in subsidies over several years beginning in 2020. Another would delay the beginning of the phase-in for two years, having it take effect in 2021 rather than 2019 as the House had proposed.
However, Broaddus and Park point out that within just a few years, the difference in the impact of the various versions of the law would be practically indistinguishable, and by 2027, just six years after taking effect, the coverage losses from the proposal incorporating the two-year delay would be equal to about 97 percent of the number who gained coverage under the expansion, barely better than the 1 percent remaining under the original plan.
In addition, they note, it wouldn’t do much to ameliorate states’ fiscal woes, either.
“[B]y 2025, the cost shift to states would be almost as large under the delayed implementation approach as under the current version of the AHCA. In states that chose to freeze their expansion enrollment, enrollment would fall by more than 66 percent by 2023 and by more than 90 percent by 2025.”
Meanwhile, one of the critics of the House Republican plan, Senator, Susan Collins of Maine, told the Portland Press Herald that she likes what’s happening in Indiana. Indiana, like Maine, did not expand Medicaid, but it did receive a federal waiver from the Obama administration to expand the program to those earning up to 138 percent of the federal poverty level.
In that case, states can charge modest premiums (in Indiana, it’s $25 a month, for which they get also get dental and vision coverage) for a family of four. Collins believes that paying into Medicaid means people will use the system more wisely.